Healthcare organizations invest a lot of time, energy and money into collecting patient feedback. Most use standardized measures like HCAHPS or patient reported outcome measures (PROMs). However, research shows that healthcare organizations struggle at incorporating the voice-of-the-patient to facilitate positive change in the patient experience.
A recent NEJM Catalyst Insights Council survey found that 73% of the survey respondents reported that incorporating patient feedback in a way that systematically improves care is a major barrier to truly capturing the patient’s voice. And while 66% of them considered measuring and improving the patient experience to be a strategic priority, only 18% think their organization has been able to implement patient feedback in a way that has improved the system.
The NEJM Catalyst Insights Council survey brought to light several emerging trends in capturing the voice-of-the-patient:
- Using PROs increases patient satisfaction, transparency and increases population-level data.
- Resistance to incorporating PROs stems from the science of measuring and defining the right outcomes, clinician buy-in and patient buy-in.
- The top barriers of implementing a patient feedback system are difficulties in implementing feedback in a systematic way, difficulty in patient’s understanding healthcare delivery and the cost associated with surveying.
When we break this down, we realize that benefits far outweigh the costs. We believe that patients will provide feedback if they feel their care team will use their voice in a meaningful way. And that the increase on healthcare consumerism and the pressures on the patient experience can we addresses with technological advances and the availability of health information.
An additional gap between the current state and desired outcomes may exist simply in the question sets each organization chooses for their measurements. Today patients are openly talking on social media and leaving reviews on online forums like Yelp and Google. These forums are unstructured and offer an unbiased, unsolicited view of their patient experience. While this feedback is unstructured and unsolicited, it is critical for the reputation of the organization to keep the finger on the pulse of what the patient population is saying about them online. If the questions an organization is asking their patients are not aligned with what patients are posting in external forums, then maybe it is time to reconsider the questions that are being asked.
The key to managing unstructured data is to mute out the noise and find the signal. Artificial Intelligence (AI) can sort through the unstructured to find trends and signals. This means for the first time in history, we can now quantify the qualitative, unstructured comments in a meaningful way. This means that we don’t necessarily have to ask standardized questions to find the answers we are seeking. We can find pulses through natural language to better understand the voice-of-the-patient. Once your organization has the right tools in place, then you can truly turn unstructured patient feedback into actionable insights that drive operational excellence.
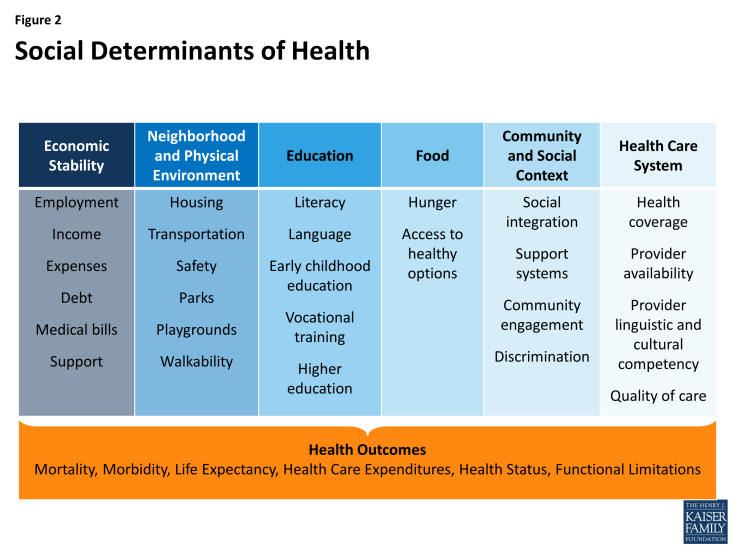
Are wait times, crowded parking lots and room temperature the most important thing to patients? What about the social determinants to health? Does your question set take into consideration social determinates that may play a role in outcomes? There are a number of delivery and payment reform initiatives within Medicaid address the diverse needs of the population served through an increased focus on social determinants of health? Social determinants of health include:
At Care Experience, we are helping healthcare organizations capture both the structured and unstructured voice-of-the-patient in a cost effective, nonintrusive way to help drive organizational excellence centered around the voice-of-the-patient.

